From stress in the workplace to the hidden toll of chronic illness, Guernsey’s workforce is facing mounting challenges.
From stress in the workplace to the hidden toll of chronic illness, Guernsey’s workforce is facing mounting challenges.
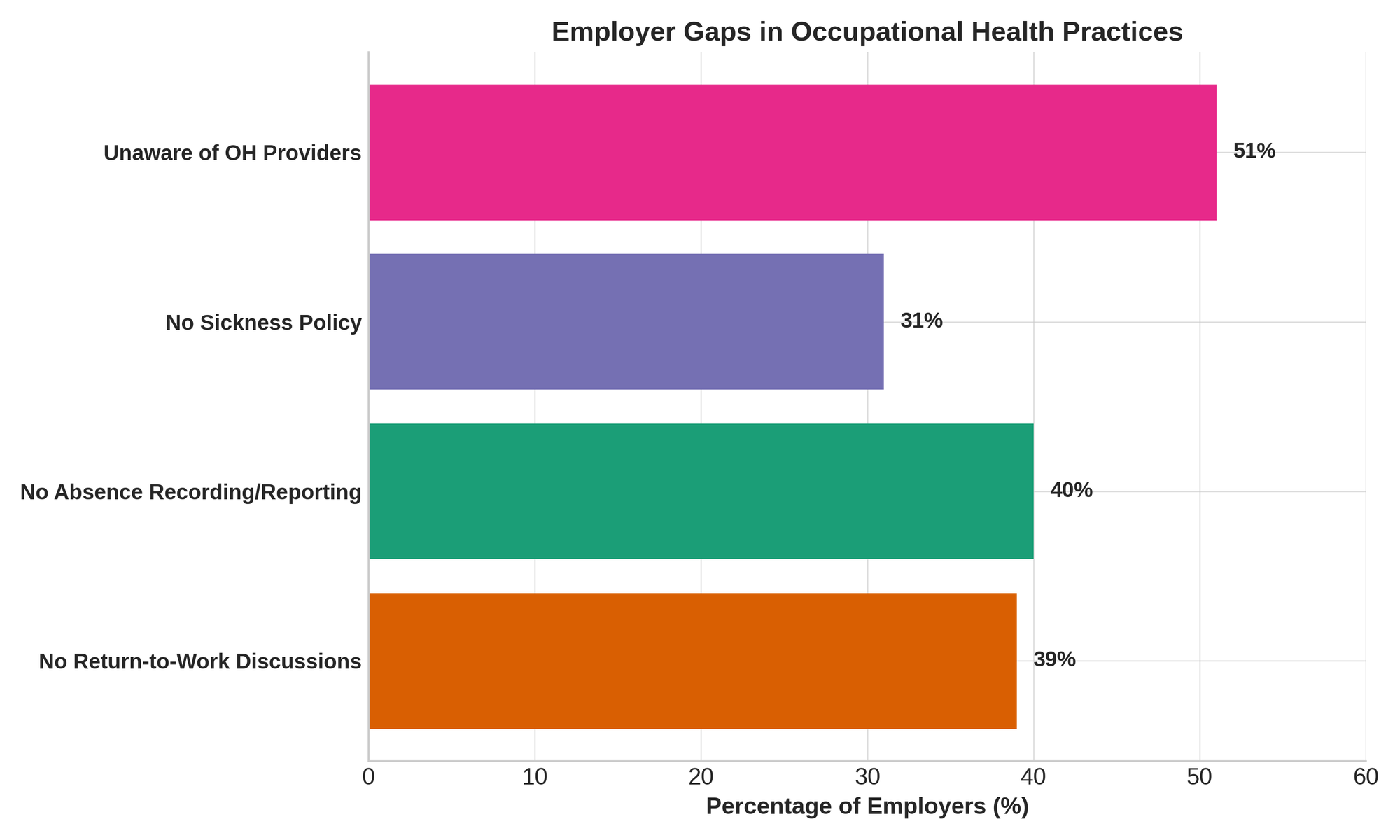
A recent employer survey has revealed key gaps in support: nearly 40% of businesses do not hold return-to-work discussions after employee illness, and 51% have never engaged with occupational health services—often due to lack of awareness.
According to the government’s new Work & Wellbeing Strategy 2025–2030, these missed opportunities for early intervention contribute to a system where too many short-term sickness claims turn into long-term incapacity.
“The Strategy recognises the value of our workforce,” said Mark Gannon, Service Lead – Benefits & Work Support for Social Security.
“We know there are lots of good practice and initiatives happening in our workplaces, but some employers may not have the support they need. This is an exciting opportunity to work across government, employers, and the community to help create a diverse, inclusive, and healthier workforce.”
The stakes are high. Expenditure on incapacity-related benefits has climbed to £31 million annually, while a shrinking working-age population and rising pension-age demographic threaten the island’s economic resilience.
The Strategy warns that unless Guernsey improves how it supports people to stay in or return to work, the burden on health, social services, and businesses will only increase.
The Cost of Ill Health
Social Security data shows that roughly 30% of benefit claims stem from mental health conditions, and another 30% from musculoskeletal (MSK) issues—both often treatable or manageable with timely support.
But long delays in accessing help, combined with outdated workplace policies, turn treatable conditions into long-term challenges.
The longer someone remains off work, the harder it becomes for them to return. After 12 months, the chances drop dramatically. And it’s not just personal; for businesses, frequent staff turnover and absenteeism lead to mounting hidden costs—lost productivity, retraining, and reduced morale.
The Mental Health Flashpoint
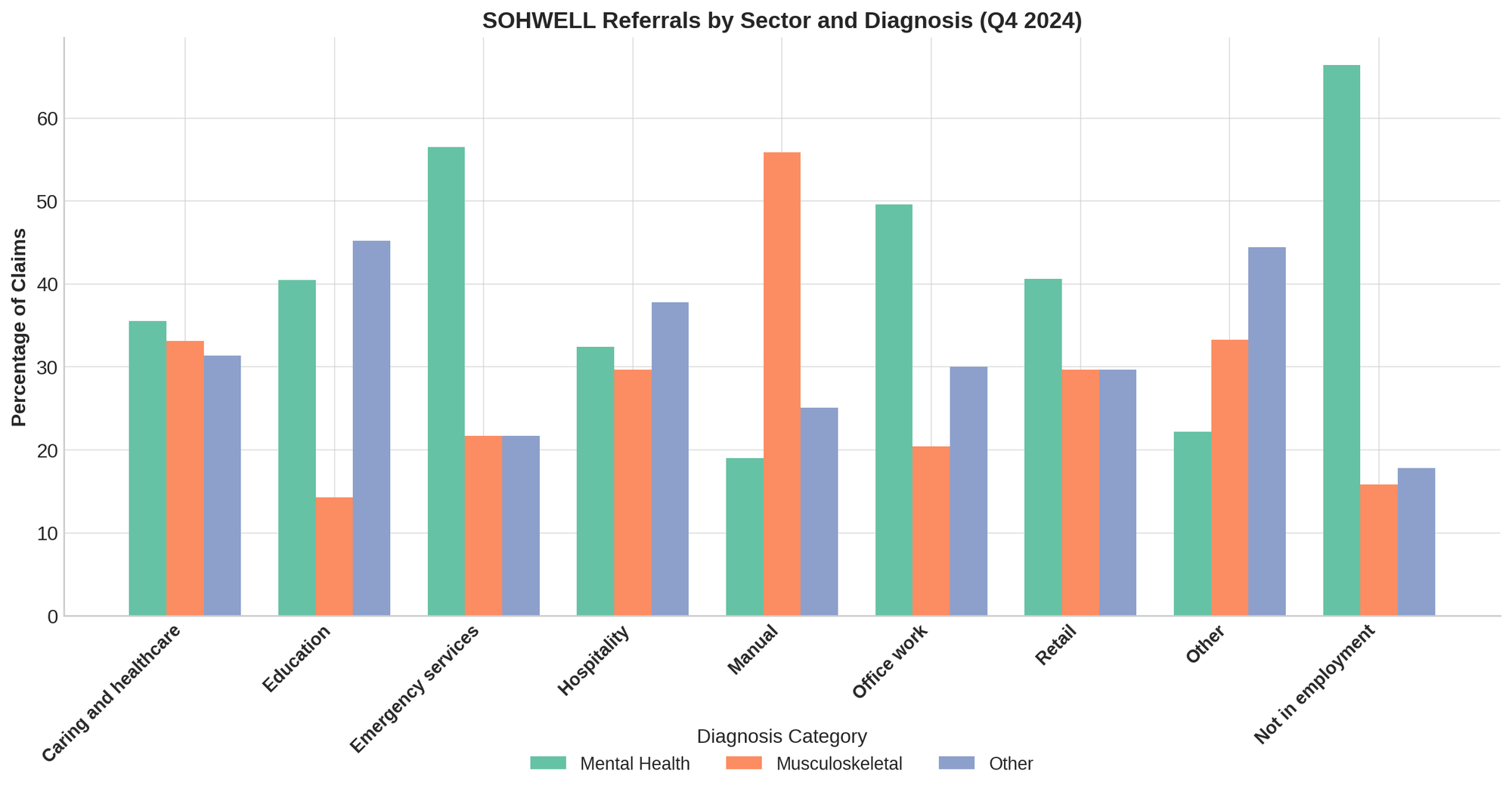
Perhaps most revealing is the surge in mental health-related claims. A decade ago, mental health made up around 23.5% of short-term claims. Now it’s 30%. Of the 1,206 cases referred to SOHWELL case managers in 2024, nearly half (503) involved mental health diagnoses.
These are not easily resolved. SOHWELL case managers report that mental health cases are more complex, requiring personalised support and careful coordination. But the return on investment is clear—where early intervention occurs, 65% of cases return to employment, and many do so on flexible or phased schedules.
Dr Bob Gallagher, Medical Adviser to the Committee for Employment & Social Security, said:
“Not being in work can have a negative effect on our health so, in most cases, it's important that patients see a return to work as part of their recovery. Within primary care I'm hearing positive stories about how the SOHWELL Programme is supporting recovery by facilitating a return to work. This Strategy is an extension to that.”
The Demographic Squeeze
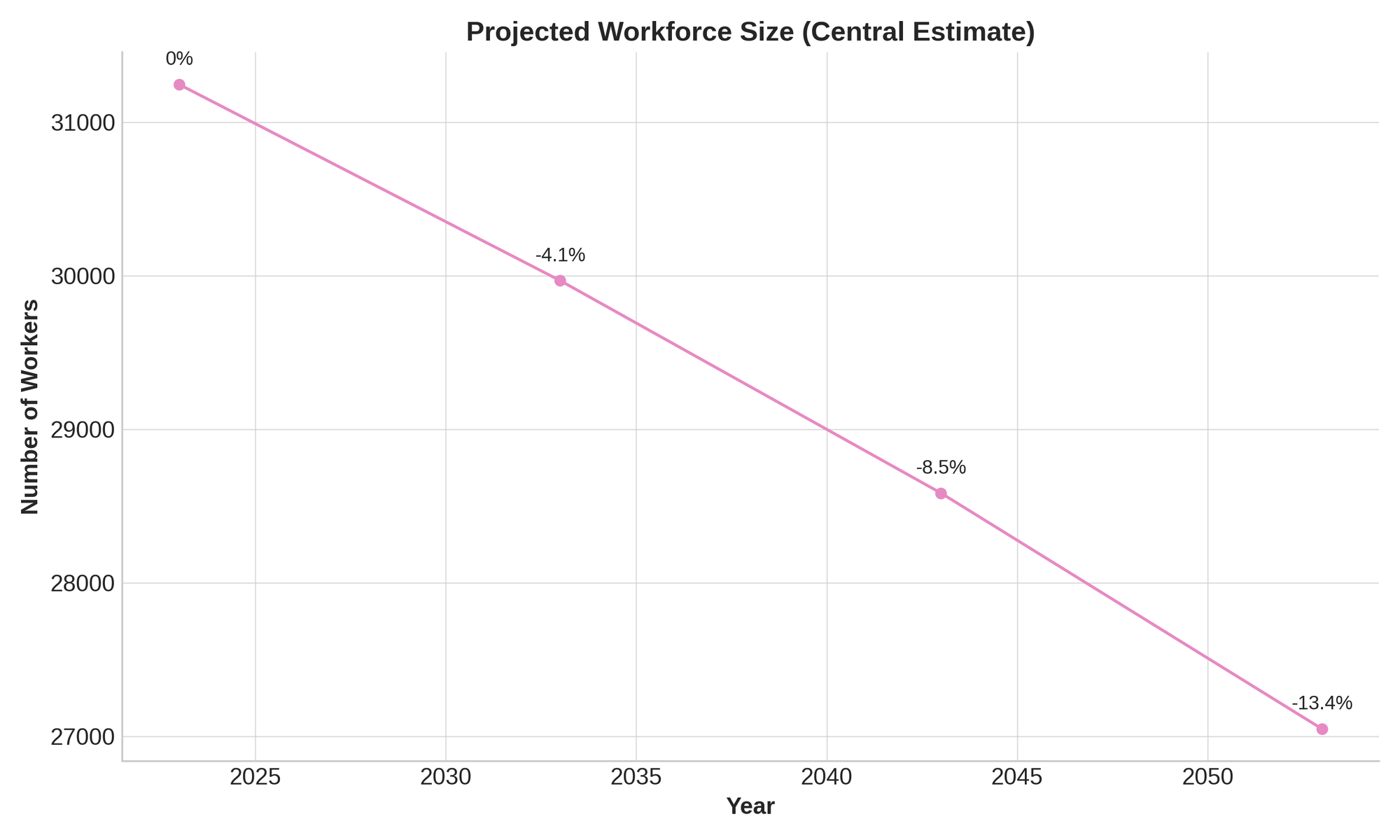
Beyond the health crisis lies a demographic one. Guernsey's working-age population is in decline. Projections show a 4.1% reduction by 2033, and 8.5% by 2043 under current trends. Meanwhile, those aged over the States pension age are expected to grow rapidly—particularly the 85+ cohort, which will double by 2049.
Even under optimistic migration scenarios, Guernsey needs to do more with less. That means keeping people healthier for longer and ensuring those with chronic conditions aren’t left behind.
At present, Guernsey residents live to an average age of 83.4 years—but only 63.6 years in good health. The Strategy’s goal? To extend not just life expectancy, but healthy life expectancy by transforming the workplace into a site of wellbeing, rather than stress and decline.
Inside the Strategy: A 3-Pillar Plan
The Work & Wellbeing Strategy 2025–2030 is built around three key pillars: Community Awareness, Prevention & Early Intervention, and Effective Services.
1. Community Awareness
At its core, the Strategy calls for a cultural shift. Too many people—and employers—still see illness and work as mutually exclusive. That has to change. The first step is education.
- Directory of Services: A community-wide directory of occupational health services will be created and publicised. Half of employers currently don’t know what’s available locally.
- Toolkits for Employers: Free resources, online guides, and training courses will help businesses—especially small ones—navigate topics like stress management, discrimination law, and reasonable adjustments.
- Workplace Accreditation: The government is exploring a voluntary scheme to recognise best practice in workplace wellbeing.
- Tackling Stigma: A campaign to reframe the conversation from “What can’t you do?” to “What can you do?” will accompany this rollout.
2. Prevention & Early Intervention
This pillar is the Strategy’s engine. Rather than wait for people to fail at work due to ill health, the plan invests early—before conditions become disabling.
- Mid-Life 'MOTs': A pilot programme will trial voluntary health assessments for people in mid-career, helping identify risks early and guiding people to re-train or adjust as needed.
- MSK Interventions: MSK conditions are often preventable and treatable with the right advice. Early support will reduce recurrence and long-term absences.
- Recruitment Grants: Financial incentives will encourage employers to hire those returning after long absences.
- Health in All Policies: A joined-up approach will integrate wellbeing into every policy area—from transport and diet to flexible working and mental health.
3. Effective Services
Making all this work means transforming the system itself.
- Digital Medical Certificates: Moving away from paper will speed up referrals, reduce delays, and enable earlier support.
- Training for GPs and Case Managers: Medical professionals will get new tools to assess work capability—not just diagnose—and better connect with rehabilitation services.
- Integrated Case Management: Teams will include physiotherapists, mental health professionals, and other specialists for a more holistic support model.
What Has Already Been Achieved
The Strategy builds on several years of groundwork laid by the SOHWELL Programme (Supporting Occupational Health & Wellbeing). Phases one and two have already delivered:
- A new medical certificate design focused on capability, not disability
- Over 120% increase in gradual return-to-work arrangements from 2023 to 2024
- Training for GPs on the link between work and health
- Better communication between doctors and case managers
- Positive feedback from users, including cancer survivors, the self-employed, and mental health claimants
In 2024 alone, 1,206 claims were managed by SOHWELL case workers. Of the 966 resolved, 65% returned to work, and many did so on a phased or supported basis.
Deputy Peter Roffey, President of the Committee for Employment & Social Security, described the vision behind the Strategy:
“Our workplaces play a pivotal role in shaping not just the economic success of our islands, but also our collective health and wellbeing. And in turn, our health and wellbeing have a significant impact on our work and productivity. A healthy workforce is the foundation of a thriving economy and must be seen as a long-term investment in our future.
“Through this Strategy, we are transforming the way we approach work rehabilitation for people who have a health condition—by shifting the narrative to focus on what people can do rather than what they can't.”
A Strategy for All of Us
The Work & Wellbeing Strategy recognises that improving workplace health is everyone’s job. Government, healthcare, employers, and employees all have a part to play.
Whether it's a small business adapting a role to support an older worker, a GP using new training to aid a patient’s recovery, or a policymaker embedding wellbeing into public services—the Strategy envisions a network of support that enables people to thrive at work, not just survive it.
Measuring Success
Key performance indicators include:
- Increased uptake of work rehabilitation services
- Fewer sickness claims converting into long-term incapacity
- Higher employer participation in wellbeing initiatives
- Rising numbers of gradual, successful returns to work
Behind the metrics is a simple but powerful philosophy: good work supports good health, and good health supports a thriving society.
Looking Ahead
As the Strategy enters its third phase, one thing is clear: work and wellbeing are no longer separate conversations. They are two sides of the same coin—and Guernsey is making a bet that investing in one will strengthen the other.



Comments ()